Diabetes, a chronic condition that impacts how the body processes blood sugar (glucose), affects millions in the United States. Whether recently diagnosed or living with it for years, understanding its causes, symptoms, and treatment options can improve management and quality of life. Here is more information on this condition, including causes, symptoms, and treatment options:
What Is Diabetes?
Diabetes is a condition where the body cannot effectively regulate blood glucose levels. This happens either because the pancreas does not produce enough insulin or because the body’s cells fail to respond to insulin properly. Insulin helps move glucose from the blood into the cells, where it is used as energy.
Two types of diabetes include:
- Type 1 Diabetes occurs when the immune system attacks and destroys insulin-producing cells in the pancreas.
- Type 2 Diabetes, the most common form, develops when the body becomes resistant to insulin or when the pancreas fails to produce sufficient insulin.
What Causes It?
The causes vary depending on the type, but genetic, environmental, and lifestyle factors can contribute. Type 1 diabetes is believed to result from autoimmune reactions that destroy insulin-producing cells. While this is likely influenced by genetic predisposition, environmental triggers, such as viruses, may also play a role.
Type 2 diabetes is closely linked to obesity, sedentary lifestyles, and genetic predisposition. Excess weight and fat distribution can interfere with the body’s ability to process insulin. This leads to insulin resistance and eventually diabetes.
What Are the Symptoms?
Recognizing the symptoms early is key for timely intervention. Common signs include:
- Increased thirst and frequent urination
- Unexplained weight loss
- Blurred vision, caused by high blood sugar
- Slow-healing wounds and frequent infections
If you experience any of these symptoms, consult a healthcare professional for testing and diagnosis.
What Does Treatment Involve?
Diabetes is a chronic condition that can be effectively managed. Treatment may involve a combination of medical interventions and lifestyle changes. Approaches are tailored to each individual based on the type and severity of diabetes.
Diabetes Education
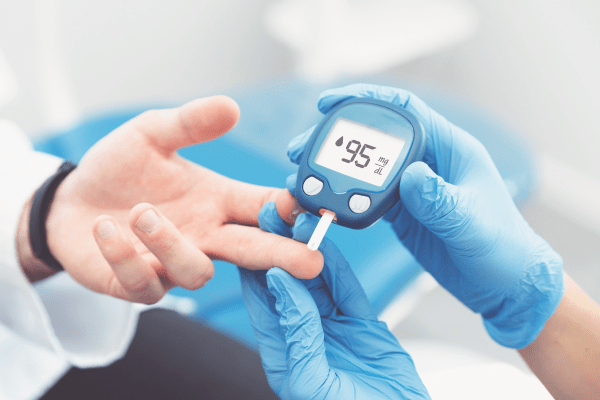
Education is a fundamental part of management. Learning about blood sugar monitoring, recognizing patterns, and understanding treatment plans helps individuals take control of their condition. Certified educators guide patients through this process, helping them develop skills necessary for effective management.
Nutrition Counseling
Nutrition counseling helps individuals understand how food influences their blood sugar levels. Strategies such as carbohydrate control and creating healthy meal plans enable individuals to maintain stable glucose levels throughout the day. Including a wide variety of vegetables, lean proteins, and whole grains is encouraged.
Exercise and Weight Management
Physical activity is an integral part of diabetes treatment. Exercise improves insulin sensitivity, helps regulate blood sugar levels, and supports overall health. Individuals may benefit from a personalized exercise plan catered to their fitness levels.
Insulin and Medications
Insulin therapy is often required for those with Type 1 diabetes. It may also be prescribed for those with advanced Type 2 diabetes. Other medications can help control blood sugar levels by improving the body’s insulin response or reducing glucose production.
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) is an effective tool for evaluating blood sugar trends in real-time. CGM devices alert individuals to fluctuations in blood sugar levels. This allows patients to make informed adjustments to diet, activity, or medication.
See a Specialist Today
Diabetes treatment involves a combination of education, lifestyle adjustments, and medical interventions. By adopting an informed and proactive approach, individuals can maintain better control over their condition and live healthier lives. Schedule a consultation with a specialist to learn more today.
- The Role of Internal Medicine in Managing Diabetes
- The Diverse Specializations Within Ophthalmologists and Their Impact on Eye Health
- Exploring the Role of Sports Medicine in Injury Prevention
- Understanding the Different Types of Hernias and Their Symptoms
- How Internal Medicine Helps When Managing Chronic Conditions